Wednesday, November 25, 2009
HOLIDAY SEASON STRESS & Healthy Chiropractic Lifestyle Choices
health to take a few simple steps to reduce the stress and
strain of this active time. The added rush of holiday observances
with the ongoing worries so many are experiencing
with economic concerns, weather-generated challenges,
and international conflicts, can pose very real
challenges to people everywhere.
Resolve to make healthier choices as you move through your day: to slow down, breathe
deeply, recognize the need for more patience, get adequate rest, and plan ahead will all help
reduce the stress of overlapping demands and last-minute efforts. Make a special point for
time and space to enjoy and explore these special holiday opportunities to share in meaningful
ways with your friends, colleagues and family members.
STABILIZE TRANSPORT:
Carrying your holiday responsibilities with care—from packages
to people—is vitally important. Both everyday activities and special
holiday travel plans call for healthy choices.
• Lift items with forethought and size up your load;
bend at the knees rather than flexing forward and just bending
at the hips. Holding the object close to your body and
maintaining a slight arch in your lower back helps the strong
leg muscles do the work, also supports loads as you lift.
• Shifting your posture helps offset prolonged
standing. Postural fatigue from shopping, entertaining or
cooking for extended periods—reduce by alternately elevating
1 foot on a chair rung/foot rest, shifting muscle loading.
• Adjust your travel strategies. Placing a pillow or
folded towel behind the small of the back can help maintain
the arch and support the rest of the body properly, relieving
the discs and joints of the spine from unnecessary pressure.
In addition to fastening your seat belt, car trips should include
adjusting the headrest to align with your head, at least
up to ear level.
• Get adjusted. Chiropractic adjustments optimize your
peak potential and help you maintain momentum.
BALANCED CHOICES:
Additional weight in the abdominal region could put 10
pounds or more stress on the lower back, forcing the pelvis
and torso to shift and cause changes in spinal balance,
leading to spinal misalignments (known as subluxations)
and malfunction in body systems.
• Avoid repeated heavy eating during holidays feasts
and avoid extra desserts and snacks, to prevent adding extra
weight. Loading on extra food can stress the digestive
system; carrying extra weight adds strain on supporting
structures of the spine and nervous system.
• What you eat is as important as how much
you eat. More evidence is accumulating that indicates
how including more fresh fruits and vegetables, along with
limiting starches and using low-sodium, low-sugar recipes,
are essential aspects of healthy eating.
• Make a helpful move to work off what you eat.
Taking even a 15-20 minute stroll after a big holiday meal
can help ease post-feast discomfort and burn some calories.
Fitness research findings indicate you can burn up to 100
calories in a 30-minute walk!
A P u b l i c I n f o r m a t i o n S e r v i c e f r o m y o u r
D o c t o r o f C h i r o p r a c t i c
a n d t h e I n t e r n a t i o n a l
C h i r o p r a c t o r s A s s o c i a t i o n
Monday, November 16, 2009
Ten Worst Breakfast Cereals
 New research confirms what consumers have long known -- most breakfast cereals advertised to children are full of sugar.
New research confirms what consumers have long known -- most breakfast cereals advertised to children are full of sugar. Cereals marketed to kids have 85 percent more sugar, 65 percent less fiber and 60 percent more sodium than those aimed at adults. In fact, the least nutritious cereals are often the most heavily marketed to children, such as Reese's Puffs, Corn Pops, Lucky Charms, Cinnamon Toast Crunch and Cap' n Crunch.
Some cereals with the poorest ratings even have health claims on the box.
San Francisco City Attorney Dennis Herrera has written a letter to the CEO of Kellogg’s, demanding evidence that Cocoa Krispies really "helps support your child's immunity" as it purports to do on the front of the box.
Cocoa Krispies are 40 percent sugar by weight. A Kellogg's company spokesperson, Susanne Norwitz, argued that Kellogg's Krispies cereals provide consumers with 25 percent of their daily value of vitamins A, C, and E.
Kellogg began making the immunity claims about Cocoa Krispies in May, however as of November 4 said they’re pulling the claim from the box.
Meanwhile, the average preschooler sees 642 cereal ads a year on TV. Most are for types with the worst nutrition ratings.
According to Cereal FACTS (Food Advertising to Children and Teens Score), which was developed based on the best available science, in consultation with a steering committee of experts in nutrition, marketing, and public health, the 10 worst breakfast cereals based on nutrition score are:
- Kellogg - Corn Pops (or Pops) - Chocolate Peanut Butter
- Quaker - Cap'n Crunch - w/ Crunchberries
- Kellogg - Special K - Chocolatey Delight
- Kellogg - Special K - Blueberry
- General Mills - Reese's Puffs
- General Mills - Fiber One - Caramel Delight
- Kellogg - Cocoa Krispies - Choconilla
- General Mills - Golden Grahams
- General Mills - Cinnamon Toast Crunch
- Kellogg - Corn Pops
November 14 2009 | 47,196 views
Sources:
ChiroHealth
http://www.acatoday.org
Friday, November 13, 2009
Obese Teens at Increased Risk for Multiple Sclerosis
November 12, 2009 — Young people with excess body weight may be at heightened risk for more than type 2 diabetes mellitus and cardiovascular disease. Researchers are now reporting that overweight teens may also be at risk for multiple sclerosis later in life. Their work appears in the November 10 issue of Neurology.
"We initially undertook this study because our previous work suggests that insufficient vitamin D nutrition is associated with an increased risk of multiple sclerosis, and other studies have shown overweight and obese individuals have lower vitamin D levels than normal weight individuals," lead investigator Kassandra Munger, ScD, from the Harvard School of Public Health in Boston, Massachusetts, told Medscape Neurology.
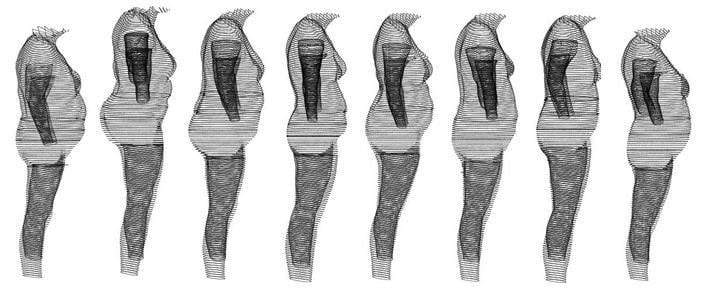 |
| Those who were already obese by age 18 had double the risk for MS. These illustrations represent a BMI of 30 or more. |
"Our hypothesis was that obesity would be associated with an increased risk of multiple sclerosis," Dr. Munger explained. "That adolescent obesity rather than childhood or adulthood obesity was associated with disease is consistent with the body of literature suggesting that exposures during adolescence may be particularly important in determining multiple sclerosis risk."
The mechanism relating obesity to multiple sclerosis is not known. Low vitamin D is one theory. Another hypothesis is that the effects of obesity are mediated by a low-grade chronic inflammatory state. Adipose tissue secretes numerous adipokines and cytokines that influence immune system function, including leptin and interleukin 6, both of which have been shown to reduce regulatory T-cell activity.
Investigators studied more than 238,000 women from the Nurses' Health Study. During 40 years of follow-up, researchers confirmed 593 cases of multiple sclerosis.
Participants provided information on weight at the age of 18 years and height and weight at baseline. They also selected illustrated silhouettes that represented their body size at the ages of 5, 10, and 20 years.
In age-adjusted analyses, women with a body mass index (BMI) of 30 kg/m2 or higher at the age of 18 years had a much greater risk of developing multiple sclerosis. This association persisted after further adjusting for smoking, latitude of residence at the age of 15 years, and ethnicity.
Multiple sclerosis risk among women who were overweight, but not obese, at the age of 18 years was only moderately increased.
Relative Risk of Multiple Sclerosis for Body Mass Index at Age 18 Years
| Body Mass Index, kg/m2 | Multivariate-Adjusted Relative Risk (95% CI) |
| <18.5 | 0.96 (0.73 – 1.27) |
| 18.5 – <21 | 1 [Reference] |
| 21 – <23 | 1.13 (0.91 – 1.40) |
| 23 – <25 | 0.97 (0.72 – 1.31) |
| 25 – <27 | 1.44 (0.87 – 2.39) |
| 27 – <30 | 1.40 (0.92 – 2.14) |
| >30 | 2.25 (1.50 – 3.37) |
Women who reported having a larger body size at the age of 20 years also had a 2-fold increased risk of multiple sclerosis compared with women who reported a thinner body.
There was also a suggestion of an increased risk associated with being heavier during childhood; however, the researchers note that reported body size at 5, 10, and 20 years of age was highly correlated.
"This is the first study to show an increased risk of multiple sclerosis among obese female adolescents," Dr. Munger said. "It will be important to replicate these findings. However, we know that obesity is associated with many poor health outcomes, and encouraging a healthy weight among all adolescents is very important to overall health."
Encourage a Healthy Weight
During a Medscape Medical News expert interview in April, Laura Hayman, PhD, from the College of Nursing and Health Sciences at the University of Massachusetts in Boston, emphasized the importance of combating childhood obesity. "The cornerstone is, of course, therapeutic lifestyle change targeting dietary intake and physical activity with consideration of the child’s growth and developmental needs," said Dr. Hayman.
The American Academy of Pediatrics recommends a staged approach, including members of a multidisciplinary team necessary for changing behaviors. Dr. Hayman says members often include nurses, behavioral scientists, dieticians, and exercise physiologists.
"Effective multidisciplinary weight management programs incorporate principles of behavior change and motivational interviewing to help the child lose weight. These programs ensure that the child feels comfortable with the principles of weight management and feels good about self and provide positive reinforcement so that the child can say, 'Yes, I can lose this weight.'"
Positive reinforcement is key, but another study published in this month's issue of the Journal of General Internal Medicine suggests that the higher a patient's BMI, the less respect physicians had for them.
Lack of Respect for Heavier Patients
Mary Margaret Huizinga, MD, from Johns Hopkins University, Baltimore, Maryland, and lead author of the study, says she came up with the idea for the research from her experiences working in a weight loss clinic.
She said that by the time patients left the clinic they would "be in tears, saying 'no other physician talked with me like this before'" and had failed to listen.
"Many patients felt like because they were overweight, they weren’t receiving the type of care other patients received," Dr. Huizinga said in a news release. Her team studied 238 patients and 40 physicians. The average BMI of patients was 32.9 kg/m2.
This study was paid for by the National Institute of Neurological Disorders and Stroke. Dr. Kassandra Munger reports that she received funding from the Consortium of Multiple Sclerosis Centers and the National Multiple Sclerosis Society.
Pain Control Recommeded for Newborns
November 11, 2009 — Feeding and breast-feeding newborns are found to be the most effective methods of pain relief during heel-lancing, according to the results of a prospective study reported in the November issue of Pediatrics.
"Pain experience can alter clinical outcome, brain development, and subsequent behavior in newborns, primarily in preterm infants," write Amir Weissman, MD, from Technion-Israel Institute of Technology in Haifa, Israel, and colleagues. "The aims of this study were (1) to evaluate several simple, commonly used methods for pain control in newborns and (2) to evaluate the concordance between behavioral and autonomic cardiac reactivity to pain in term neonates during heel-lancing."
During heel-lancing for routine neonatal screening of phenylketonuria and hypothyroidism, 180 term newborn infants were randomly selected to 1 of 6 groups: (1) control (no intervention for pain relief); (2) sucking without feeding; (3) holding by mother; (4) ingestion of oral glucose solution; (5) feeding with oral formula; or (6) breast-feeding. Response to pain was assessed with the Neonatal Facial Coding System score; duration of crying; and autonomic variables determined from spectral analysis of heart rate variability before, during, and after heel-lancing.
Compared with newborns in any of the 5 intervention groups, those in the control group with no pain intervention had the greatest levels of pain manifestation. Breast-feeding or feeding with oral formula appeared to be most effective vs all other groups, based on the lowest increase in heart rate (21 and 23 beats per minute, respectively, vs 36 beats per minute; P < .01), neonatal facial score (2.3 and 2.9, respectively, vs 7.1; P < .001), cry duration (5 and 13 seconds, respectively, vs 49 seconds; P < .001), and the lowest decrease in parasympathetic tone (–2 and –2.4, respectively, vs 1.2; P < .02).
"Any method of pain control is better than none," the study authors write. "Feeding and breast-feeding during heel-lancing were found to be the most effective methods of pain relief."
Limitations of this study include low sensitivity of the pain assessment methods, large variability of newborn response to painful stimuli, and the subjective nature of interpreting these data.
"Neonatal pain prevention is the expectation of the parents and should be the goal of the medical staff; therefore, family members or staff may be recruited to help during these procedures, and nursing mothers should be encouraged to breastfeed during the procedure," the study authors conclude. "If family members believe that they cannot withstand the procedure, hear their infant crying, or see the heel-lancing, then bottle-feeding seems to be a good alternative."
The study authors have disclosed no relevant financial relationships.
Pediatrics. 2009;124:e921-e926.


